Cancer treatment for women: Possible sexual side effects
Cancer treatment can cause physical changes that make having sex more difficult.
By Mayo Clinic Staff
Sex might be the last thing on your mind as you start thinking about cancer treatment options and cope with the anxiety that comes with a cancer diagnosis.
But as you start to feel more comfortable during cancer treatment and afterward, you'll want to get back to a "normal" life as much as you can. For many women, this includes resuming sexual intimacy.
An intimate connection with a partner can make you feel loved and supported as you go through your cancer treatment. But sexual side effects of cancer treatment can make resuming sex more difficult.
Find out if you're at risk of sexual side effects during and after cancer treatment and which treatments can cause these side effects.
Who's at risk of sexual side effects?
Women with the greatest risk of sexual side effects include those being treated for:
- Bladder cancer
- Breast cancer
- Cervical cancer
- Colon cancer
- Endometrial cancer
- Ovarian cancer
- Rectal cancer
- Uterine cancer
- Vaginal cancer
- Vulvar cancer
Treatment for any cancer carries the risk of causing physical changes to your body that can alter your body image and your sexuality. But having cancer also affects your emotions, no matter what type of cancer you have. For instance, you may feel anxious and worn out about your diagnosis, your treatment or your prognosis. These emotions can also affect your attitude toward sex and intimacy with your partner.
What sexual side effects are most common?
The treatment you receive and your type and stage of cancer will determine whether you experience sexual side effects. The most commonly reported side effects among women include:
- Difficulty reaching climax
- Less energy for sexual activity
- Loss of desire for sex
- Pain during penetration
- Reduced size of the vagina
- Vaginal dryness
Not all women will experience these side effects. Your doctor can give you an idea of whether your specific treatment will cause any of these.
How does cancer treatment cause sexual side effects?
Cancer treatments that are more likely to cause sexual side effects include the following.
Chemotherapy
Many women experience a loss of libido during and after chemotherapy. Often the side effects of the treatment — such as fatigue, nausea, hair loss, and weight loss or gain — can make you feel unattractive.
Side effects usually fade soon after treatment ends. But it may take time to rebuild your self-confidence to bring back your desire for sex.
Chemotherapy can cause a sudden loss of estrogen production in your ovaries. This can lead to symptoms of menopause, such as a thinning vagina (vaginal atrophy) and vaginal dryness, both of which can cause pain during penetration.
Ask your doctor about what you can expect from your chemotherapy drugs, as some can cause either a temporary or permanent menopause.
Depending on your cancer type, your doctor may prescribe estrogen replacement therapy — also called hormone therapy for menopause — to reduce the sexual side effects you experience. Topical estrogen creams applied to the vaginal area also can be used. However, women with hormone-sensitive breast or ovarian cancer should carefully discuss any type of hormone therapy with their doctors. Many of these conditions may respond to treatments that do not use hormones.
Chemotherapy can also damage tissues in your body, including the vagina. This damage can cause sores and may increase your risk of infection. It can also cause fatigue or increased bleeding. During this time, your doctor may advise you to avoid sexual intercourse, or you may not feel the desire for sex.
Radiation therapy
Sexual side effects related to radiation therapy are most common in women receiving treatment to the pelvic area.
Radiation to the pelvis causes:
Damage to the ovaries. The amount of damage and whether it's permanent depends on the strength and site of your radiation treatments.
Damaged ovaries don't produce estrogen. This causes menopause and its related signs and symptoms, such as vaginal dryness or hot flashes. If you've already been through menopause, you likely won't experience such symptoms.
Changes in the vaginal lining. Radiation therapy can irritate healthy tissue in its path. This can cause the lining of your vagina to become inflamed and tender. Penetration during sex may be uncomfortable during treatment and for a few weeks afterward.
As the lining of your vagina heals, it may become thickened and scarred, causing your vagina to tighten and resist stretching during penetration. Your doctor might recommend using a vaginal dilator to prevent scar tissue from forming after radiation.
Talk to your doctor about what you can expect from your specific radiation treatments. Some side effects may be preventable. For instance, surgery to relocate your ovaries to another part of your body might spare them from the damage of radiation and preserve your fertility. Ask your doctor about your options.
Surgery
Whether surgery affects your ability to have sex will depend on the type of cancer you have, where it's located and its size.
Surgical procedures that are likely to cause sexual side effects include:
Radical hysterectomy. One treatment for cervical cancer may be a radical hysterectomy to remove the uterus and related ligaments, as well as the cervix and part of the vagina. A shortened vagina usually doesn't change your ability to have sex, though it may take some adjustment.
The surgeon may also remove the ovaries during this procedure. If you're premenopausal when your ovaries are removed, you'll experience menopause.
Radical cystectomy. In this operation for bladder cancer, the surgeon removes your bladder, uterus, ovaries, fallopian tubes, cervix, the front wall of your vagina and your urethra.
Your surgeon reconstructs your vagina, though it may be shorter or narrower than it was before surgery. This can make sex painful. If you haven't been through menopause, removal of your ovaries will cause menopause.
Abdominoperineal (AP) resection. AP resection may be used if you have colon or rectal cancer. Your surgeon removes your lower colon and rectum. Without the cushion of the rectum, you might experience pain in your vagina during penetration.
Some women who have an AP resection also have their ovaries removed. If you're premenopausal, this will cause premature menopause.
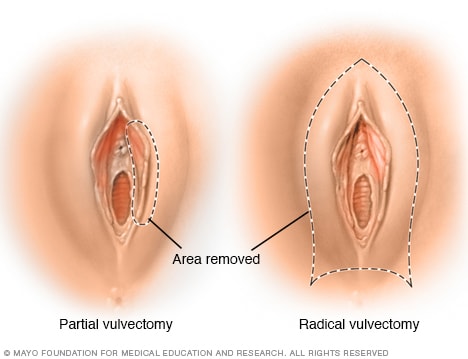
- Vulvectomy. You may undergo vulvectomy if you have cancer of the vulva. Your surgeon removes the entire vulva, including the inner and outer lips, as well as the clitoris. These play a major part in sexual arousal in women. Removing the vulva and the clitoris can make the area less sensitive and make it harder for you to reach orgasm.
In addition, some operations may require placement of an opening (ostomy) that allows stool or urine to collect in a bag that attaches to your body. Wearing an ostomy bag may make you feel self-conscious and unattractive. Ostomy therapists and specialized clothing can help boost your self-confidence.
Hormone therapy
If you have a hormone-sensitive cancer, you might receive hormone-blocking therapy through medications, such as tamoxifen or aromatase inhibitors, or through surgery, such as removal of your ovaries (oophorectomy).
If your cancer is sensitive to hormones, these hormone-blocking therapies can be effective in shrinking or killing the cancer and can decrease the chance of a cancer recurrence.
Both medications and surgery for hormone therapy cause menopausal signs and symptoms, including hot flashes and vaginal atrophy and dryness. Removing your ovaries causes permanent menopause. There are many different treatments that can lessen these side effects, so discuss them with your health care team.
Side effects of hormone therapy medications usually wear off after you stop taking them. Women taking hormone therapy for cancer usually take these drugs for five years or more.
What can you do to regain your sexual function?
Knowing what sexual side effects to expect before you begin your cancer treatment can help you be more prepared to deal with them.
If you experience sexual side effects, find out as much as you can about what's impeding your sexual function. This will help you feel more in control and help guide you to treatment options.
You may also want to:
Talk with your health care team. It can feel uncomfortable to talk about sexual side effects. Though talking about sex can be awkward, you're not likely to find a solution if you don't let someone know what you're experiencing.
Write down your questions if it makes you feel more comfortable. In addition, your doctor may be embarrassed or hesitant to talk about sex. If this is the case, ask to be referred to a specialist or seek support from other members of your health care team, such as nurses and counselors.
Talk with your partner. Let your partner know what you're experiencing and how he or she can help you cope. For instance, you might find that using a lubricant eases your vaginal dryness or changing positions helps you avoid genital pain during sex.
Together you may find solutions to ease you back into a fulfilling sex life.
Explore other ways of being intimate. Intercourse isn't the only option for closeness with your partner. Consider spending more time together talking, cuddling or caressing.
Connecting in other ways might help make you feel more comfortable and less anxious about the sexual side effects you're experiencing.
Talk with other cancer survivors. Your health care team might be able to steer you to a support group in your town. Otherwise, connect with other cancer survivors online.
If you're embarrassed about discussing sex face to face with strangers, the online environment provides you anonymity. Start with the American Cancer Society's Cancer Survivors Network.
It may simply take time for you to regain your sexual function after cancer treatment. While that can be frustrating, remember that if you had a positive and satisfying sex life before cancer, you'll likely resume that after your treatment.









.jpeg)

